A Recent Publication Summary:
A Summary of Trends in Liver Transplantation for Autoimmune Liver Diseases: A Canadian Study
A Summary of Trends in Liver Transplantation for Autoimmune Liver Diseases: A Canadian Study
by Kristian Stephens
Can J Surg 2022 October 12; 65(5). doi: 10.1503/cjs.012121
The following is a summary of the October 12, 2022 publication of this study in the Canadian Journal of Surgery. The paper was written by: Carla F. Murillo Perez, Tommy Ivanics, Marco P.A.W. Claasen, Peter Yoon, David Wallace, Nazia Selzner, Gideon M. Hirschfield, Bettina E. Hansen, and Gonzalo Sapisochin.

This Canadian based study looked at the outcomes of 1070 adults (age ≥ 18 years) who had a liver transplant in Canada from 2000 to 2018 because of an auto immune disease. These were patients having either primary biliary cholangitis (PBC), primary sclerosing cholangitis (PSC), autoimmune hepatitis (AIH) or two conditions (PBC–AIH or PSC–AIH). Data was collected from five Canadian transplant hospitals in British Columbia, Alberta, Ontario, and Nova Scotia. This study was done to help identify: (1) gaps and (2) areas for potential health care improvement in Canada.
Of the 1070 liver transplant surgeries for autoimmune diseases during the study period, 489 (45.7%) were for PSC, 341 (31.9%) for PBC, 220 (20.6%) for AIH and 20 (1.9%) were for those with more than one disease. During this study period, 5722 adult liver transplant surgeries had occurred at these five hospitals. Regardless of the disease type, the overall number of primary liver transplant surgeries increased over time, from 251 in 2000 to 349 in 2018. There was a significant increase in the total number of procedures for PSC over the study period. There was no significant difference in the total number of procedures for PBC or AIH, with an average of 18 for PBC and 12 for AIH across all years.
In contrast, the proportion of patients who received a liver transplant for PSC remained stable over the study period (average of 9%), whereas the proportion of those who received a liver transplant for PBC or AIH decreased over time. The increase in the total number of transplant surgeries for PSC occurred in a stable proportional trend over time. This may have been due to the increase in the overall number of transplant surgeries for other indications. This suggests that the burden of PSC related end-stage liver disease may be increasing over time in Canada.
Graft type, donor age, bilirubin level, creatinine level and MELD score at the time of transplantation were similar across the three disease groups. The MELD score at the time of transplantation increased over time. Specific overall PSC patient data from this study is in the table below.
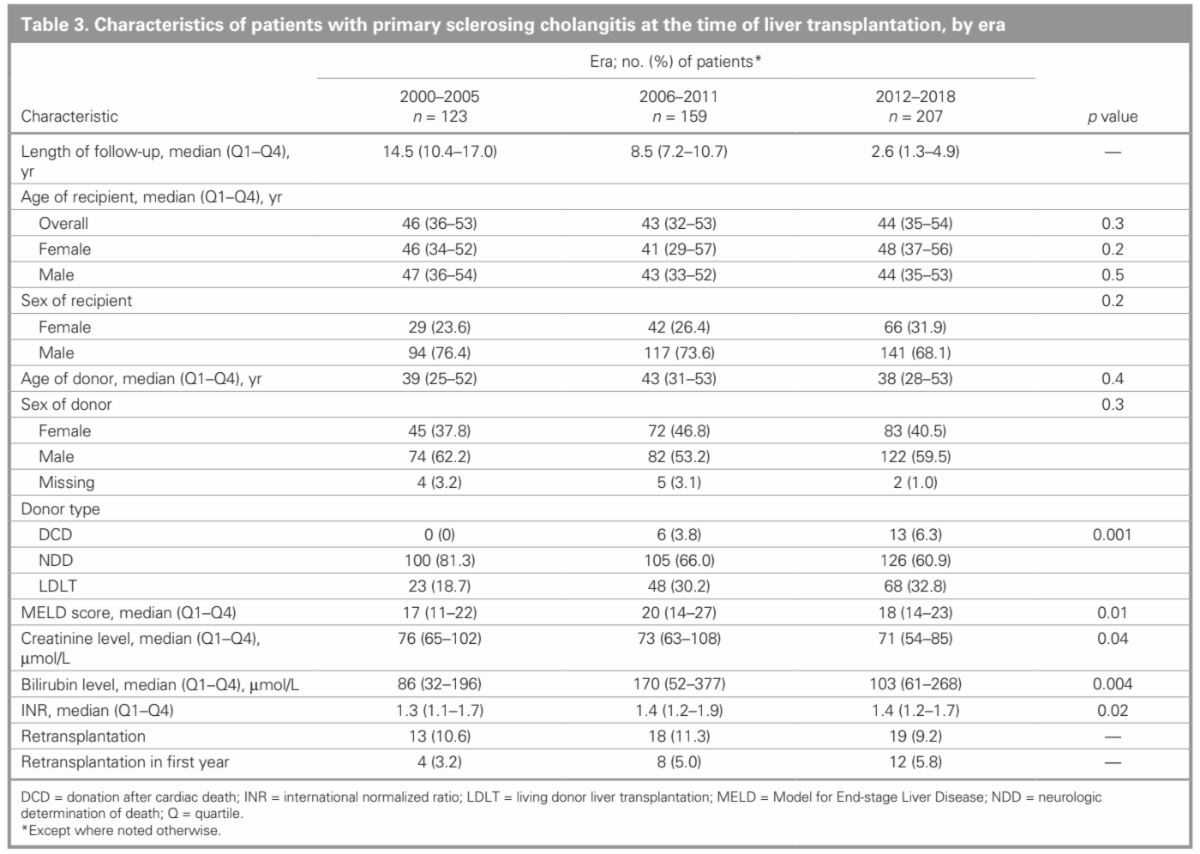
Table 3 from Trends in liver transplantation for autoimmune liver diseases: a Canadian study, Canadian Journal of Surgery
Post transplantation survival improved significantly over time only among patients with PBC. Although recipient age differed over time for the PBC and PSC groups, it was stable for the AIH group. No significant differences in the overall incidence of graft failure were observed between the liver disease types over the study period. The 5-, 10- and 15-year incidence rates of graft failure were 11.4%, 11.9% and 16.6%, respectively, among patients with PBC; 12.1%, 17.8% and 21.1%, respectively, among those with PSC; and 6.5%, 9.6% and 15.2%, respectively, among those with AIH.
Limitations of this study include the absence of waitlist status in the Canadian database, which prevented analysis of waitlist survival and potential changes over time, and the performance of intention-to-treat analyses. Liver transplantation procedures conducted in Quebec are not included, and this may have affected the findings from a Canadian experience perspective. There were some aspects that could not be considered, such as post transplantation immunosuppression regimens and their impact on outcomes, because the data were not available.


















