AASLD is the American Association for the Study of Liver Diseases, a professional association for doctors, scientists, and healthcare providers focused on preventing, curing, and treating liver diseases. At November 2025’s AASLD annual professional conference, several research posters highlighted work made possible through PSC Partners Seeking a Cure, PSC Partners Canada, and the PSC patient community in collaboration with researchers and other patient advocacy organizations. These posters underscore the growing role of patient voices in shaping PSC research. Some of this work is led by the research team at PSC Partners and/or is collaborative work funded wholly or in part by PSC Partners.
Why This Matters
These posters show how patient-driven data can influence research priorities, improve outcome measures, and highlight real-world challenges faced by people living with PSC. By bringing patients’ lived experiences into the scientific spotlight, your participation ensures that future therapies and clinical care are more responsive to what matters most to the PSC community. To stay informed of opportunities to contribute to research, please be sure to join the PSC Partners Patient Registry and keep your profile and email updated.
🔹 Gaps in PSC Patient Education & CCA Surveillance “Identifying Gaps in PSC Patient Education and Understanding of Cholangiocarcinoma Screening and Surveillance Practices: Results of a Multinational Patient Survey”
Lead Author: Brian T. Thorsen, Co-authors: Martine Walmsley, Susan O’Dell, Rachel Gomel, Mark Chatterley, Mary P. Vyas, Stephen J. Rossi
This multinational survey found that many people with PSC experience gaps in communication and understanding around cholangiocarcinoma (CCA) screening and surveillance. The results highlight a need for clearer, more consistent education and shared decision-making between patients and healthcare providers.

Background and Aims: People with primary sclerosing cholangitis (PSC) have up to a 20% lifetime risk of cholangiocarcinoma (CCA). CCA surveillance is challenged by the poor performance of current screening methods. We report results of a multinational patient survey to assess knowledge of CCA surveillance and patient-provider communication on CCA risk and surveillance results. The primary goal was to identify gaps in knowledge and communication in anticipation of new CCA screening tests.
Methods: A survey for adults with PSC was developed by PSC Partners and PSC Support patient organizations. Patients reported relevant medical history, CCA surveillance tests performed (MRCP, CA 19-9, ERCP), risk and results discussion, and CCA education. The data was analyzed to compare rates of proactive CCA discussion from providers by patient characteristics, region, and provider type.
Results: A total of 623 responses met screening criteria, primarily from the US (45%) and UK (31%). 31 patients reported a biliary tract cancer diagnosis (25 CCA, 6 GBC). Only 51% of patients reported proactive discussions by their provider of CCA risks and surveillance. Among patients who had a proactive CCA discussion, 56% reported having sufficient information regarding CCA, versus only 15% among those without proactive discussion (p < 0.001). Patients in North America reported a higher rate of proactive discussion than Europe (58.2% / 36.9%, p < 0.001), and rates were higher for hepatologists than gastroenterologists (55.0% / 38.3%, p < 0.001). Discussion rates were not significantly different across patient gender, age, and time since PSC diagnosis.
Annual MRCP surveillance was reported by 68% of patients, with significant differences by region and provider type. Proactive CCA discussion was strongly associated with more frequent use of annual MRCP. Regular CA 19-9 testing was reported by 36% of respondents. MRCP and CA 19-9 testing results for CCA surveillance were discussed with 27% and 72% of patients who had those tests, respectively.
Only 36% of patients felt they had adequate CCA information; the majority seeking information from online search, followed by patient organizations and their care team. Patients consistently reported significant anxiety and fear regarding CCA risk and the need for a reliable, non-invasive screening test.
Conclusion: The results show high variability in discussion of CCA risk and test results and CCA surveillance practice in a population burdened with anxiety and fear around CCA. These results are influenced by differences in regional guidelines, healthcare systems, and the lack of highly predictive non-invasive diagnostic and prognostic tools. Promising novel biomarkers to detect early CCA and risk will impact the current routine surveillance practices and patient education needs. Appropriate global patient/provider education and communication programs should be implemented to support the use and delivery of such tests.
🔹Liver Pain in PSC “It’s More Like a Dull, Achy Pain That’s Just Constant”
Lead Author: Donna Evon, Co-authors: Lauren Wright, Laura Mkumba, Nicole Lucas, Kaya Merkler, Ricky Safer, Joanne Hatchett, Rachel Gomel, Stephen Rossi, Mark Swain, Sasha Deutsch‑Link, Bryce Reeve
This poster explored liver pain experiences in adults with PSC through in-depth interviews. Patients described a range of pain types — from dull and achy to sharp and stabbing — providing critical insights for developing PSC-specific patient-reported outcome measures for research and clinical care.

Background: An in-depth understanding of experiences with liver pain associated with chronic liver disease is virtually non-existent, especially for individuals living with PSC. The development of a PSC-specific liver pain measure suitable for clinical trials relies upon understanding key characteristics of liver pain in this population.
Methods: Adults with PSC were recruited through the PSC Partners Patient Registry and hepatology experts in the U.S. Participants were phone screened for the presence of multiple PSC-related symptoms. Purposeful sampling was used to recruit a representative sample of 17 adults for in-depth qualitative interviews about key PSC symptoms experienced in the last month, including liver pain. Interviews were conducted virtually, audio-recorded, transcribed, and analyzed using NVivo software.
Results: Ten out of 17 participants who reported liver pain as a prominent PSC symptom described their experiences in detail, while another three spontaneously mentioned liver pain during their interviews. Participants were, on average 43 years old (range: 27-65), 50% male, 60% white, 30% black, 10% Asian and 30% had inflammatory bowel disease (IBD). Participants’ experiences of their liver pain are found in the Table below. Participants described the location of PSC-associated liver pain generally in the right upper quadrant area, but said it can extend around the side and back. Eleven of 13 described liver pain as “stabbing” or “sharp.” Eight described their pain as “achy” or “dull.” The sharp/stabbing pain is typically brief, while the achy/dull pain is more persistent. All but one participant used the word “pain” to describe their sensations. Liver pain can “come and go” intermittently, happens at random, and seems
unassociated with specific triggers. Some reported pain daily, others weekly, and most reported pain occurring outside of cholangitis attacks. Participants were able to differentiate PSC-related liver pain versus abdominal pain from other causes (including IBD) based on location and type of pain, timing, response to medications, and laboratory/clinical markers. Liver pain interfered with sleep and caused anxiety, but relative to fatigue and brain fog, it appears to interfere less with daily functioning. Participants tended to “push through it.”
Conclusion: Dull/achy and sharp/stabbing liver pain may be more frequent and severe in symptomatic adults with PSC than previously recognized. These in-depth qualitative findings will inform the development of a de novo PSC-specific liver pain measure, inclusive of heterogeneity of experiences, and suitable for future PSC research studies.
🔹 Cognitive Impairment (“Brain Fog”) in PSC “This Is Not Normal; Understanding Cognitive Impairment Through Qualitative Interviews With Adults With PSC to Inform Measure Development”
Lead Author: Donna Evon, Co-authors: Kaya Merkler, Laura Mkumba, Lauren Wright, Nicole Lucas, Ricky Safer, Joanne Hatchett, Rachel Gomel, Stephen Rossi, Patrick Smith, Mark Swain, Sasha Deutsch‑Link, Bryce Reeve
Through interviews, researchers documented how PSC affects cognitive function, including memory, focus, and mental clarity. These insights will support the creation of better tools to measure cognitive symptoms in PSC clinical research.
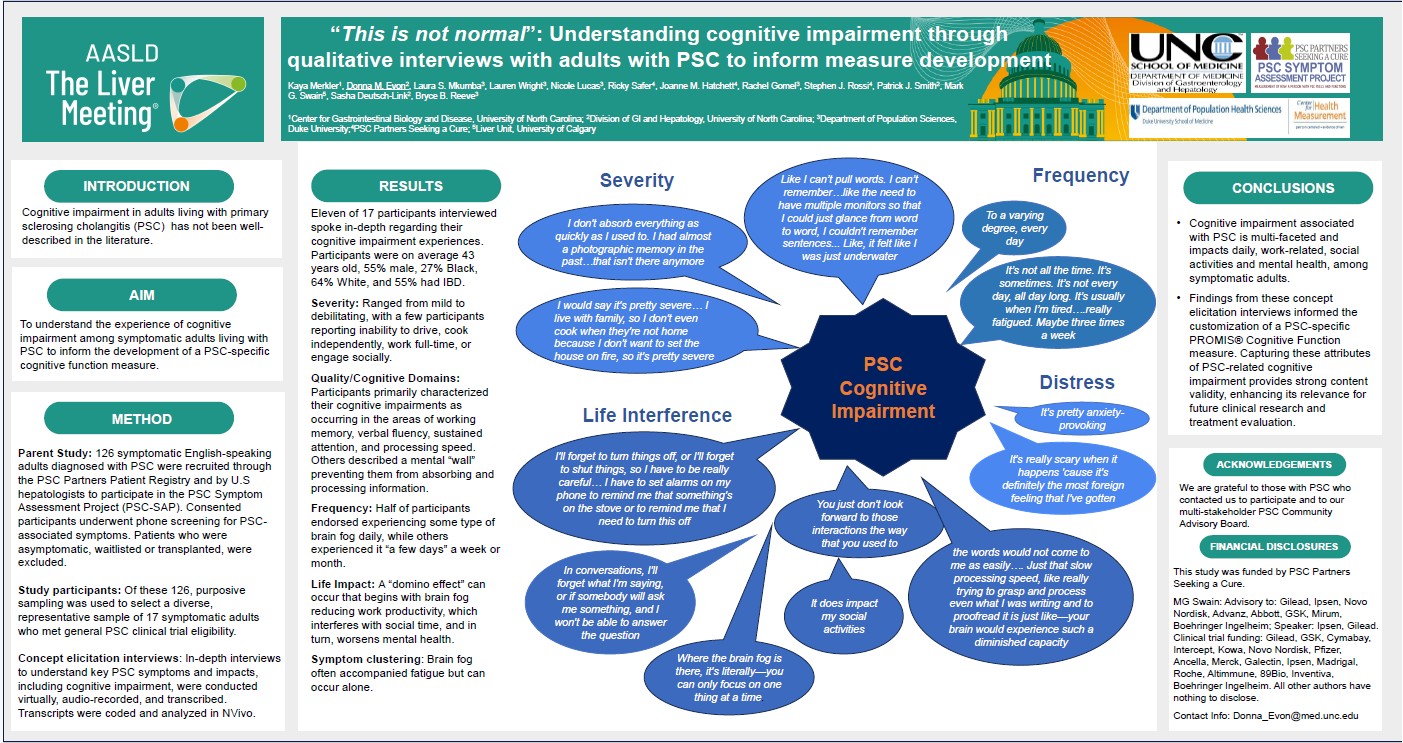
Background: Understanding cognitive impairment experiences for adults living with PSC is essential for the development of PSC-specific, patient-reported outcome (PRO) measures that accurately reflect their real-world impact. Cognitive impairment (“brain fog”) in PSC is under-recognized yet can be frequent and debilitating, and is differentiated from hepatic encephalopathy.
Methods: Adults were recruited through the PSC Partners Patient Registry and PSC hepatologists in the U.S and screened for a range of PSC-related symptoms. Purposeful sampling was used to select 17 participants for in-depth, individual interviews focused on key symptoms, including cognitive impairment. Interviews were conducted virtually, audio-recorded, transcribed, and analyzed using NVivo software.
Results: Eleven out of 17 participants were interviewed regarding their experience with cognitive impairment. Participants were on average 43 years old (range: 27- 65), 55% male, 27% Black, 64% White, and 55% had inflammatory bowel disease. The Table below provides participants’ illustrative quotes aligned with cognitive domains and life impacts. Severity ranged from mild to debilitating, with a few participants reporting inability to drive, cook independently, work full-time, or engage socially. Participants primarily characterized their cognitive impairments as occurring in the areas of working memory, verbal fluency, sustained attention, and processing speed. Others described a mental “wall” preventing them from absorbing and processing information. Half of participants endorsed experiencing some type of cognitive impairment on a daily basis, while others experienced it “a few days” a week or month. A “domino effect” can occur that begins with cognitive impairment reducing work productivity, which cuts into social time, and in turn, worsens mental health. Cognitive impairment. often accompanied fatigue, but
reportedly can also occur alone. Most participants were able to differentiate PSC-related cognitive impairment from other causes based on association with severe fatigue, improvements with ERCPs and lactulose, and worsening during cholangitis attacks.
Conclusion: PSC cognitive impairment is multi-faceted and impacts daily, work-related, and social activities among symptomatic adults with PSC. These findings will inform the customization of a PSC-specific PROMIS® Cognitive Function measure with strong content validity, enhancing its relevance for future clinical research and treatment evaluation.
🔹 Symptom Burden Profiles in PSC “Symptom Profiles Among Adults With PSC Identifies Low, Moderate and High Burdened Groups”
Lead Author: Donna Evon, Co-authors: Kaya Merkler, Chelsea Anderson, Joanne Hatchett, Ricky Safer, Rachel Gomel, Sasha Deutsch‑Link, Christopher Bowlus, Bryce Reeve
Using data from the PSC Partners Patient Registry, this study identified distinct symptom burden groups — from low to high impact. Symptoms like fatigue, itch, pain, and cognitive difficulties often cluster, helping researchers understand the diverse ways PSC affects daily life and why tailored approaches to treatment are important.
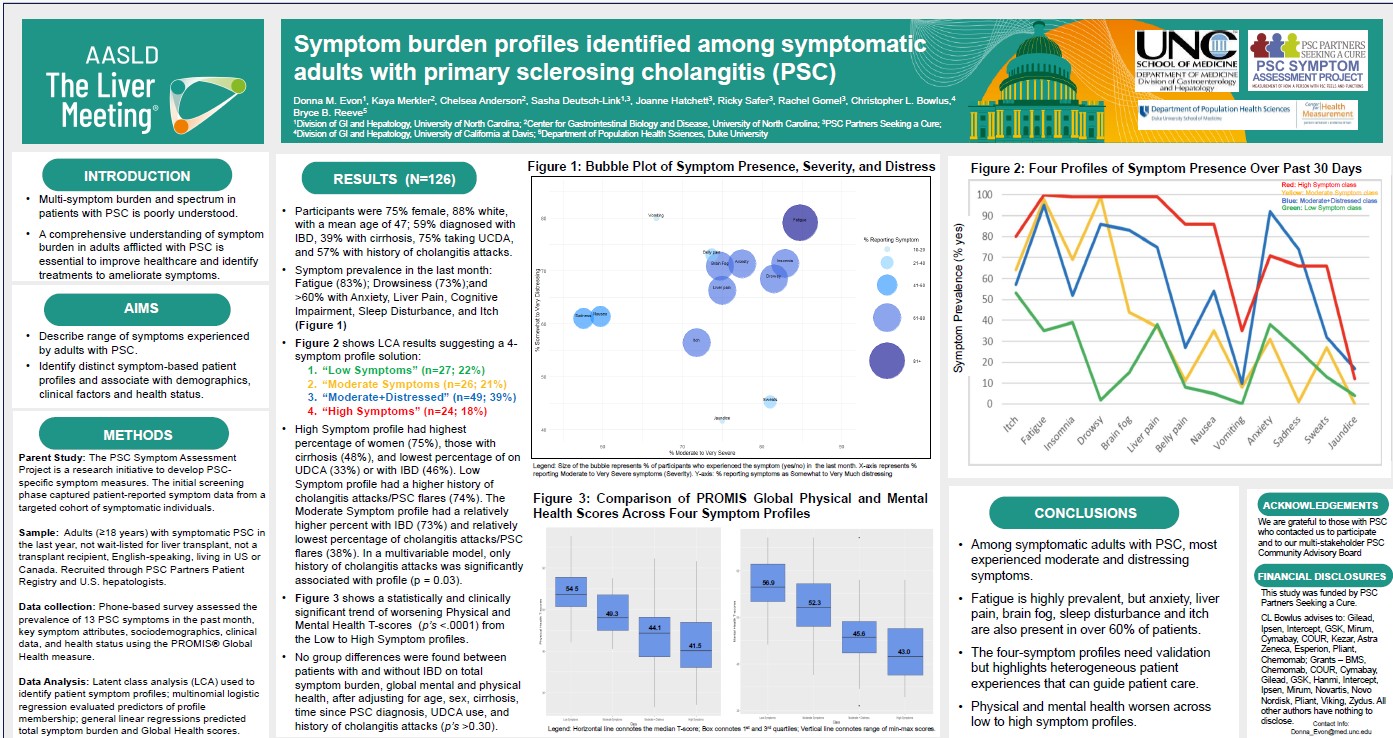
Background: Patient-reported symptoms of PSC are not well documented. The study’s aim was to understand the prevalence of PSC symptoms and identify distinct symptom profiles and their association with demographic and clinical characteristics among symptomatic adults.
Methods: Adults were recruited through the PSC Partners Patient Registry and PSC hepatologists in the U.S. Individuals were eligible if they were 18 or older, symptomatic in the last year, and not waitlisted or a transplant recipient. Individuals engaged in a phone survey that screened for the presence (yes/no) of 13 PSC-associated symptoms in the last month. Sociodemographic and medical history were self-reported. Latent class analysis (LCA) was used to identify symptom-based participant profiles based on symptom presence and participants were assigned to one symptom class. Multinomial logistic regression models were used to evaluate demographic or clinical factors associated with profile membership.
Results: Participants (n = 126) were on average 47 years old (range:20-81), 60% female, 88% white, 8% black and 3% asian, 59% had inflammatory bowel disease (IBD), 39% reported cirrhosis, 75% were taking ursodiol (UCDA), and 57% had a history of cholangitis attacks. The most prevalent symptoms in the last month included fatigue (83%), daytime drowsiness (73%), and liver pain, cognitive impairment, anxiety, sleep disturbance and itch (all 62-63%). The LCA and clinical interpretation suggested a 4-symptom profile solution: (1) “Low Symptom” class (22% of sample), (2) “Moderate Symptom” class (21%), (3) “Moderate+Distressed” class (39% of sample), and a “High Symptom” class (18%). In unadjusted models, compared to the Low Symptom class, females were more likely than males to be in the High Symptom class (OR =4.36; 95% CI: 1.31-14.51), participants taking UCDA were less likely to be in the High Symptom class (OR =0.25; 95% CI: 0.08-0.80) and those with a history of cholangitis attacks were less likely to be in the Moderate Symptom class (OR = 0.22; 95% CI: 0.07-0.70). In the multvariable model, only a history of cholangitis attacks (p = 0.03) was statistically associated with class membership. A statistically significant worsening trend was observed in PROMIS® Global Physical and Mental Health T-scores from the Low to the High Symptom classes.
Conclusion: Among symptomatic adults with PSC, over 60% report fatigue, daytime drowsiness, liver pain, cognitive impairment, anxiety, sleep disturbance and itch in the past month. The four-symptom profiles ranging from low to high burden needs validation in larger cohorts as they have clinically meaningful implications for patients’ health status and care of symptomatic individuals.
For more information about AASLD visit HERE.